UC's custom 3D-printed skull implants go global
A simplified, cost-effective method for 3D-printed components is on the horizon
By Jonathan Forbes, M.D.
Assistant Professor of Neurosurgery, UC College of Medicine
During my deployment at Bagram Air Base, Afghanistan, I saw firsthand the ramifications associated with a lack of treatment options for skull repair in developing countries.
In one case, a young boy was severely injured after reaching to pick up what he thought was a toy buried in the ground. It turned out to be one of millions of land mines left by the former Soviet Union during withdrawal from the Soviet-Afghan war. The mine exploded, and the young boy needed a decompressive craniectomy performed by military neurosurgeons to relieve pressure in the skull and save his life. He later returned for a cranioplasty, a procedure that restores the integrity of the skull with an implant. In this case, doctors used titanium mesh, a common option in countries with limited resources. Unfortunately, this material is known to be associated with an increased risk of delayed wound complications. By the time I saw the patient, the titanium mesh had eroded through his skin. He needed several additional procedures to repair the damage.
Cases like this are typical in developing countries. When patients acquire a bone defect, it is preferable in most cases to use the patient’s own bone flap. When the flap is not salvageable, synthetic materials are the next best option. Here in the United States, third-party companies produce anatomically precise patient-specific cranial implants using the patient’s CT scans. However, the cost for this type of implant is often prohibitive in countries with developing economies. Options for calvarial reconstruction in these regions are limited in many regards. Titanium mesh implants do not readily conform to many three-dimensional defects and can be associated with wound contracture, poor cosmesis (cosmetic appearance) and delayed wound erosion. Polymethyl methacrylate (PMMA), or bone cement, implants have to be manually shaped or directly poured into the defect. The cosmesis of this form of implant is often limited and depends on the ability of the surgeon to shape the implant appropriately before the cement hardens.
Developing a more affordable option
Is there a better option available? Researchers at the University of Cincinnati believe that with utilization of additive manufacturing, or 3D printing, a feasible solution may exist.
In recent years, 3D printing has become more commonplace in medical research and personal use. An entry-level 3D printer costs about one-quarter the price of a single patient-specific cranial implant (PSCI) in the United States. Etudies have demonstrated success with printing PSCIs and molds for cranioplasties. The postoperative cosmesis, in particular, has been excellent.
Why then has this solution not been widely utilized by surgeons in developing countries? The answer lies in the time commitment required to master the computer software necessary to transition from CT imaging to a file ready for printing. The lengthy training process and the necessary hours at the computer to generate each mold is more than enough to deter a busy surgeon.
With knowledge of this obstacle, I have partnered with Sam Anand, Ph.D., professor of mechanical engineering in UC's College of Engineering and Applied Science, to research a way to simplify the process for surgeons in developing countries. The goal is to make this technology freely available to neurosurgeons around the world.
The goal is to make this technology freely available to neurosurgeons around the world.
Dr. Jonathan Forbes, UC assistant professor of neurosurgery
The aim of the project is to create a freeware program that allows neurosurgeons to upload CT scans of patients with a skull defect with near-instantenous generation of a file ready for 3D printing. The program will be free, reproducible with minimal clinician training and anatomically accurate for the defect.
Anand’s research team has carefully constructed an algorithm for this research program with the needs of neurosurgeons in developing countries in mind. Printed implants using PMMA or titanium are the most convenient for intraoperative use but require more sophisticated printers and options for sterilization. The best option for surgeons in developing countries is a 3D printed mold that can be sterilized and allow casting of a PSCI in the operating room. Under sterile conditions in the operating room, bone cement can be injected into the mold and be ready for insertion in less than 30 minutes.

An example of a 3D-printed mold for creating a cranial implant. Photo/provided.
How does this new software program rapidly generate a file of a PSCI mold? The innovative concept behind the development of this software revolves around the utilization of the patient’s own skull as a template. The side of the skull opposite to the missing bone is mirrored onto the defect, which facilitates precise acquisition of flap margins. The Boolean difference is obtained, which generates a virtual implant. The virtual implant is then used to create a two-piece mold able to support intraoperative injection of bone cement. The final implant precisely restores the skull surface with symmetrical surface contours, ideal thickness and a seamless fit.
Making 3D-printed cranioplasty a reality
The Center for Global Design and Manufacturing at UC is collaborating with us to turn this idea into reality. Anand, the center’s director, leads a team of engineers with extensive experience in additive manufacturing and software programming. Three graduate students, Omkar Ghalsasi (M.S. student) and Vysakh Venugopal and Matthew McConaha (Ph.D. students), are working on this project under Anand’s supervision with Alice Xu, a third-year medical student at UC's College of Medicine.
Current 3D-printing technology allows the manufacture of complex-shaped parts, which is crucial in developing customized medical solutions. Due to the center’s prior expertise in developing algorithms for additive manufacturing and converting scan data to geometric models that can eventually be 3D printed, the team is able to successfully adapt these methods with some modifications to this project. It will result in a truly user-friendly end-product: users will be provided with an executable file along with instructions and installation manuals. The computational complexity of the entire process is low, enabling the installation and use of this software tool-kit in inexpensive desktops or laptops.
Through this collaboration, we hope to put the right tools in the hands of neurosurgeons—delivering hope to patients around the world through the power of science.
This article, which first appeared on UC Health, was written in conjuction with CEAS.
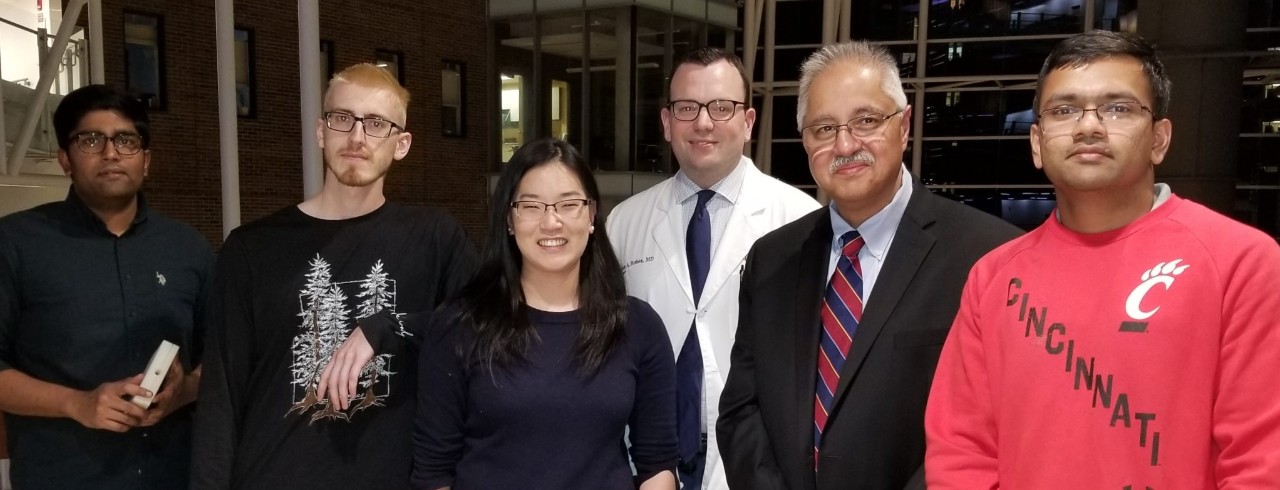
Featured image at top: The combined engineering/medical research team at UC. Photo/provided.
Next Lives Here
The University of Cincinnati is classified as a Research 1 institution by the Carnegie Commission and is ranked in the National Science Foundation's Top-35 public research universities. UC's graduate students and faculty investigate problems and innovate solutions with real-world impact. Next Lives Here.
Related Stories
Engineering doctoral student studying cyberattack prevention...
April 21, 2025
As a top graduating student in his undergraduate class, Logan Reichling came to the University of Cincinnati to further his education through the direct-PhD program in computer science. His initial connection to UC’s College of Engineering and Applied Science was through his current advisor, Boyang Wang, in an undergraduate research program. Since arriving at CEAS, Reichling has been honored with several awards, including being named Graduate Student Engineer of the Month.
UC researcher develops at-home diagnostic test for endometriosis
April 21, 2025
Katherine Burns, a University of Cincinnati researcher who has endometriosis, speaks about her journey of developing a non-invasive diagnostic test for the condition.
NEXT Innovation Scholar Charlie Harker
April 21, 2025
From strategizing with community leaders on the future of transportation solutions to collaborating with global corporate partners to dive into complex consumer insights, the NEXT Innovation Scholars (NIS) program at the University of Cincinnati empowers a new generation of leaders and problem solvers.
