MSN: Ohio legislation aims to cover dense breast screening
UC expert says current process doesn't guarantee insurance coverage, change needed
Mammogram screenings are recommended to detect early signs of breast cancer, but around 40% of women have dense breast tissue that can make cancer harder to detect through mammography.
Those with dense breast tissue can seek out tomosynthesis, an ultrasound or MRI to find any potential breast cancers, but the state of Ohio currently only requires health care providers to inform patients that their dense breast tissue "could hide abnormalities" and is "relatively normal."
A new proposed legislation, House Bill 371, would alter the required text to clarify that dense breast tissue may make it harder to find cancer through mammography and directly refer patients to seek additional screening.
The bill would also require health insurance companies to cover MRI or ultrasound screenings for patients with dense breast tissue or a family history of breast cancer.
Annie Brown, MD, assistant professor of radiology in the College of Medicine and a UC Health breast radiologist, told MSN that even in cases where insurance companies currently cover dense breast screening, like with high-risk patients, pre-authorization is required and actual coverage is not guaranteed for all patients. This may lead to patients declining the additional screenings due to concern of out-of-pocket costs.
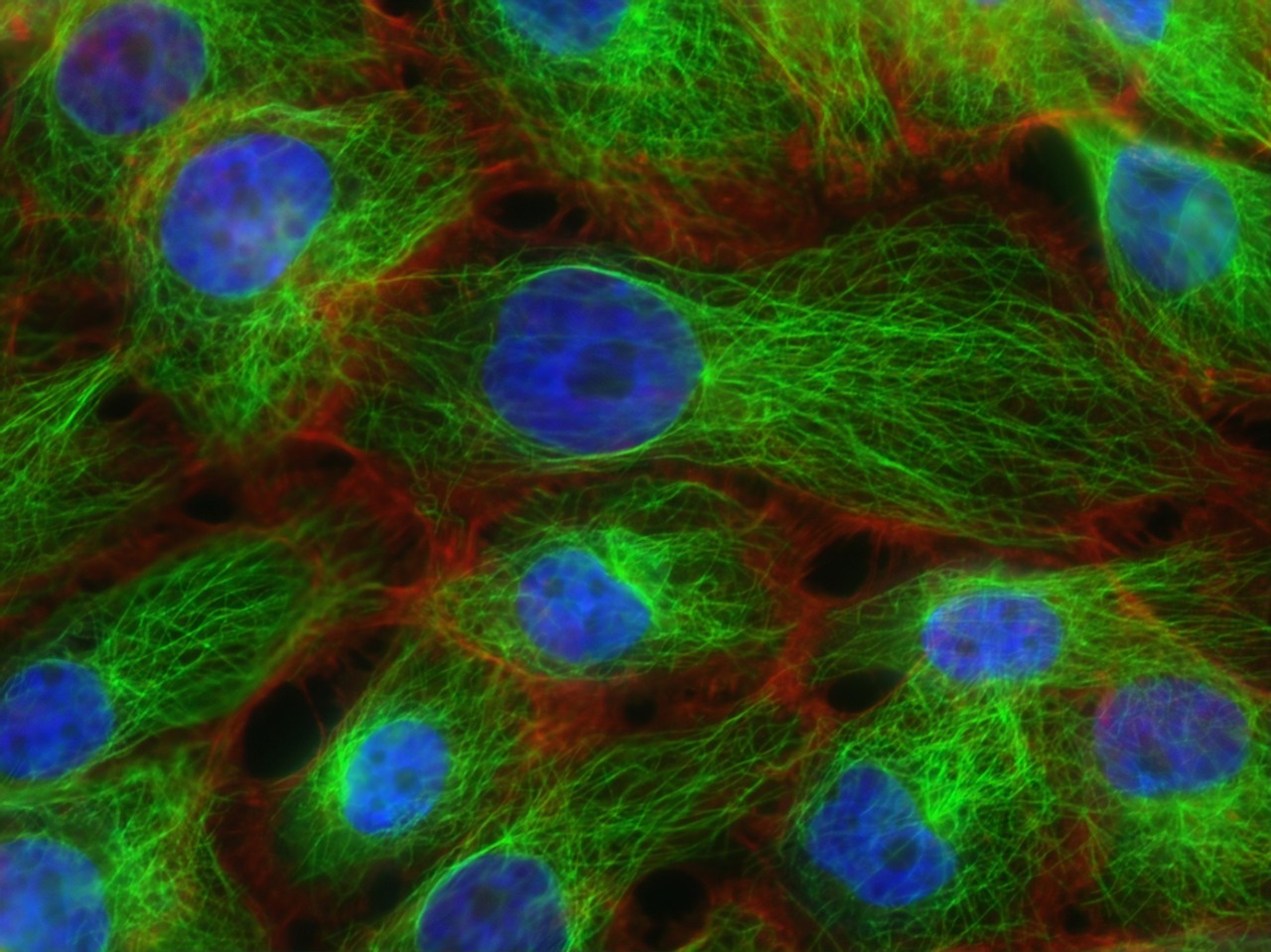
Featured photo at top of breast cancer cells courtesy of the National Cancer Institute.
Related Stories
UC professor Ephraim Gutmark elected to National Academy of...
December 20, 2024
Ephraim Gutmark, distinguished professor of aerospace engineering at the University of Cincinnati, was elected to the 2024 class of the prestigious National Academy of Inventors.
UC Law professors recognized for scholarly excellence
December 19, 2024
University of Cincinnati College of Law professors Stephanie McMahon and Andrew Mamo were recently recognized for their scholarly contributions.
ADAAPT: Growing Student Ideas
December 19, 2024
Steven Doehler, an industrial design professor at the University of Cincinnati’s College of Design, Architecture, Art, and Planning (DAAP), says he prioritizes the entrepreneurial aspect of a student's design product – which led him to create HomeGrown Studio.
