Examining how stress affects Parkinson’s disease
New models, federal funding aid UC researchers in study of motor and nonmotor symptoms
Stress can have a negative effect on anyone’s health but presents particular challenges for people with Parkinson’s disease.
Kim Seroogy, PhD, said previous research from his team has shown that chronic stress can exacerbate Parkinson’s disease and lead to degeneration of brain cells and motor functions at a faster rate.
Now, Seroogy and his research collaborators at the University of Cincinnati have received a $1.2 million grant from the U.S. Department of Defense (DOD) to examine how stress hormone receptors affect cell degeneration.
The hypothesis

Kim Seroogy, PhD. Photo/University of Cincinnati.
Seroogy, professor and director of the Selma Schottenstein Harris Lab for Research in Parkinson’s in the Department of Neurology and Rehabilitation Medicine at UC’s College of Medicine, said stress hormones activate a receptor in cells which may accelerate neuron death in areas of the brain that regulate motor and nonmotor function. The study will examine if blocking or removing these receptors can halt or even reverse cell degeneration that is worsened by chronic stress.
“Many Parkinson’s patients have high levels of stress hormones,” Seroogy said. “So we think that elevated levels of stress hormones and chronic life stress accelerates the course of their disease. If we can block that receptor, maybe that can slow the progression of the disease.”
Progress in disease modeling
Collaborator James Herman, PhD, said improved animal models that better replicate the progression of Parkinson’s disease will be crucial to better understanding the relationship between stress hormones and neuron death.
Using gene-editing technology, Herman’s lab has developed an animal model that can specifically delete the stress hormone receptors in brain cells associated with Parkinson’s.
“One of the beauties of the model is that we are able to essentially target the gene, leaving the rest of the brain unaffected,” said Herman, director of the UC Neurobiology Research Center and Flor van Maanen professor and chair of the Department of Pharmacology and Systems Physiology in the College of Medicine. “It’s a very precise manipulation. We can ask very specific questions about the role of this receptor and these important dopamine neurons that are killed off in Parkinson's disease.”
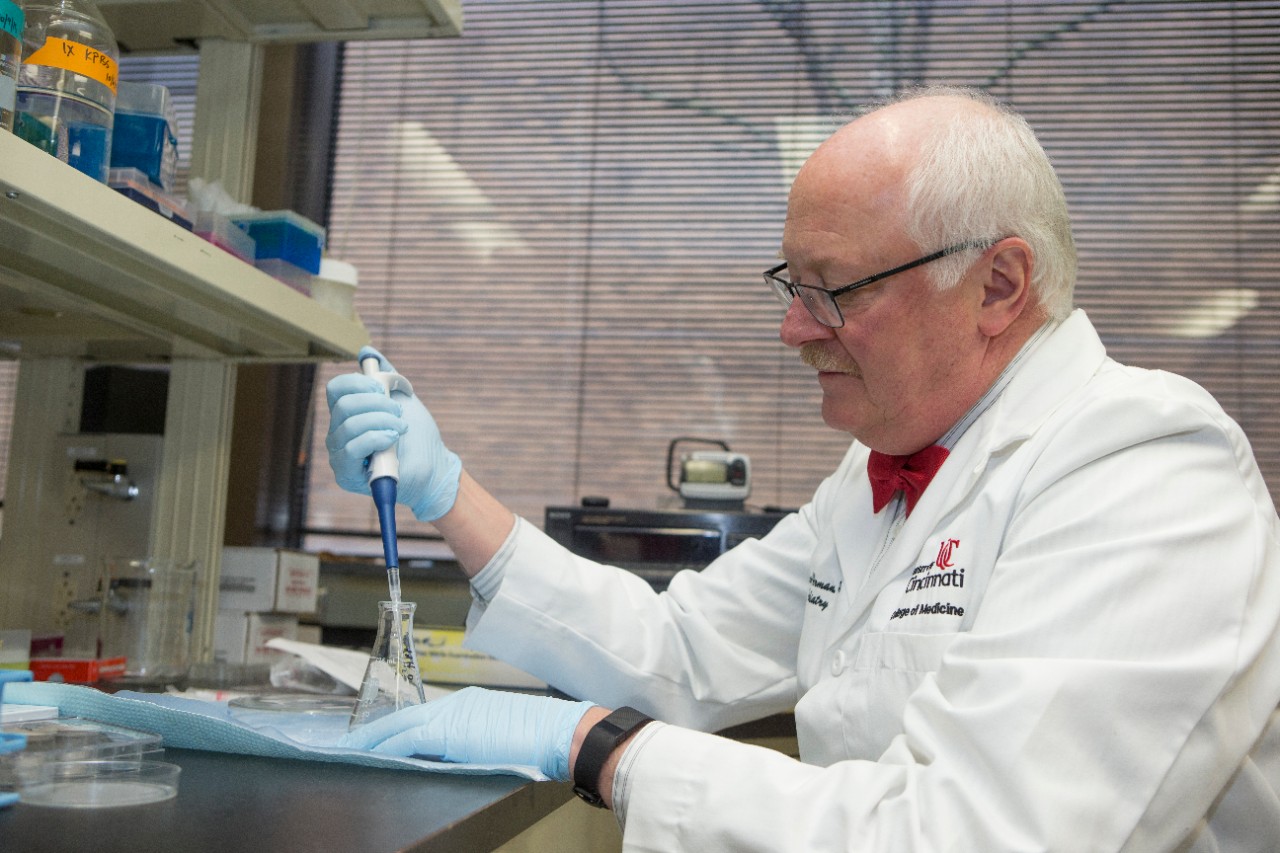
James Herman, PhD, and his colleagues have developed a new animal model that can delete stress hormone receptors in a targeted process that doesn't affect other parts of the brain. Photo/Andrew Higley/University of Cincinnati.
Seroogy will also be using a relatively new leading model that better mirrors how Parkinson’s progresses in a clinical situation over a prolonged period of time.
“Previous models produced relatively quick cell death, which is not what happens in Parkinson’s,” he said. “This newer model generates a gradual cell loss that is more clinically relevant. And importantly, by combining the two sophisticated animal models in the current study, we now have the means to understand the mechanism by which key stress hormones act on vulnerable midbrain dopamine cells to cause loss of normal function and cell degeneration ”
Nonmotor symptoms

Teresa Reyes, PhD. Photo/University of Cincinnati.
While Parkinson’s is commonly associated with the deterioration of motor functions and mobility, Herman said many patients routinely report nonmotor symptoms such as mood and cognition issues, with up to 50% experiencing depression.
“Through interacting with my clinical colleagues both in psychiatry and in neurology, it has become clear that the incidence of depression in these individuals is quite striking,” Herman said. “When we treat patients, we tend to treat the primary symptoms that you can see and put your hands on, but some of the cognitive and mood symptoms tend to get swept under the rug. If anything, this research is also going to help shed light on that particular problem.”
To test how deleting the stress hormone receptors affects cognition, Teresa Reyes, PhD, was brought into the research.
Reyes, professor in the Department of Pharmacology and Systems Physiology, specializes in detailed cognitive testing on animal models like the ones being used in this study. She will conduct assessments of the animals that test higher-order cognitive functions like attention and the ability to change how a task is completed.
“Sometimes the rules for solving a puzzle change, and an animal needs to modify their response strategy. This is known as ‘cognitive flexibility,’” Reyes explained. “In this new project, we will examine behaviors such as cognitive flexibility and attention to determine whether there are any higher-order cognitive deficits in these animals.”
Seroogy said grant reviewers noted that cognitive behavior has been understudied in Parkinson’s research, so this project presents a great opportunity to study both deficits caused by Parkinson’s in a single study.
“So it’s kind of a win-win in terms of addressing not just motor but also the debilitating nonmotor symptoms as well,” he said.
We need to let patients and their families know the importance of stress management, including cognitive behavioral therapies, hobbies, things that can kind of engage positively with the patient.
James Herman, PhD
Looking ahead
If the study shows that removing the stress receptors can stop or reverse the effects of Parkinson’s, Seroogy said next steps over the coming years could include working toward treatments through stress hormone blockers or next-generation therapeutics that target the receptors with more specificity and fewer side effects.
Herman said as the research continues, it is paramount to emphasize the importance of stress management to Parkinson’s patients since stress has been found to be a prominent factor of disease progression.
“We need to let patients and their families know the importance of stress management, including cognitive behavioral therapies, hobbies, things that can kind of engage positively with the patient,” he said.
Seroogy said prior to the current DOD grant, the research has been supported through the UC Gardner Neuroscience Institute pilot grant program and by generous philanthropy through the UC Foundation’s Kerman Family Fund for Parkinson's Research, the Parkinson’s Disease Support Network of Ohio, Kentucky & Indiana, Northern Kentucky Putting for Parkinson’s and the Morris Braun Fund. Herman credited the $25,000 pilot grant, in particular, as helping generate and test the new animal models which led to a large return on investment in the form of the DOD grant.
Seroogy said he is grateful to be part of a collaborative team.
“This is a great example of interdepartmental collaboration across different fields and different departments,” Seroogy said. “I’m a systems neurobiologist with expertise in Parkinson’s basic research, then there’s [Herman] with his expertise in stress and other behaviors, and then [Reyes] with her expertise in cognitive function. Interdepartmental collaboration clearly leads to success.”
Impact Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
This work is supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Neurotoxin Exposure Treatment Parkinson’s Program under Award No. W81XWH-21-1-0877. Opinions, interpretations, conclusions and recommendations are those of the researchers and are not necessarily endorsed by the Department of Defense. The researchers cite no conflicts of interest.
Featured photo at top courtesy of Pixabay.
Related Stories
UC celebrates record spring class of 2025
May 2, 2025
UC recognized a record spring class of 2025 at commencement at Fifth Third Arena.
Leveling up
May 2, 2025
Meet four College of Allied Health Sciences students who are advancing their education following graduation this May.
CCM welcomes new viola faculty member Brian Hong
May 1, 2025
UC College-Conservatory of Music Dean Pete Jutras has announced the appointment of Brian Hong as CCM's new Assistant Professor of Viola. His faculty appointment officially begins on Aug. 15, 2025. Hong has established a notable career as a critically acclaimed performer, inspiring pedagogue and successful music administrator. As the violist of the GRAMMY-nominated Aizuri Quartet from 2023-2025, he premiered major new works on nationally renowned chamber music series and conducted residencies at universities across the United States.
