
Omicron hit rural America harder than cities
Patients unvaccinated for COVID-19 died at twice the rate of vaccinated patients
The omicron wave of the COVID-19 pandemic in late 2021 and early 2022 spread like a grass fire in America’s densely populated cities, but led to higher rates of death in rural counties where vaccinations are lagging.
The latest study by the University of Cincinnati, published in the journal Frontiers in Medicine, revealed striking disparities in health care between urban and rural America.
“This new national study, looking back at the delta and omicron variants of COVID-19, demonstrates the power and utility of geospatial and data visualization analysis,” said co-author Neil MacKinnon, formerly dean of UC’s James L. Winkle College of Pharmacy, now provost of Augusta University.

Neil MacKinnon
“It is our hope this information might be useful for decision-makers for future public health campaigns and approaches to address pandemics.”
The United States was hit by the fourth and most severe wave of the COVID-19 pandemic through a variant known as omicron that infected even many of those who were vaccinated. Researchers relied on data from 2,417 counties to track the incidence of cases and the mortality rate per 100,000 people between Dec. 1, 2021, and Jan. 31, 2022.
They found that counties with vaccination rates of less than 40% had far higher mortality rates than counties with vaccination rates of 60% or more. The study recommended that health policymakers continue to make vaccination coverage a priority.
“Omicron spread like crazy. The daily peak of omicron infections was three times higher than the peak of delta,” said Diego Cuadros, lead author of the study and director of UC’s Digital Epidemiology Lab.
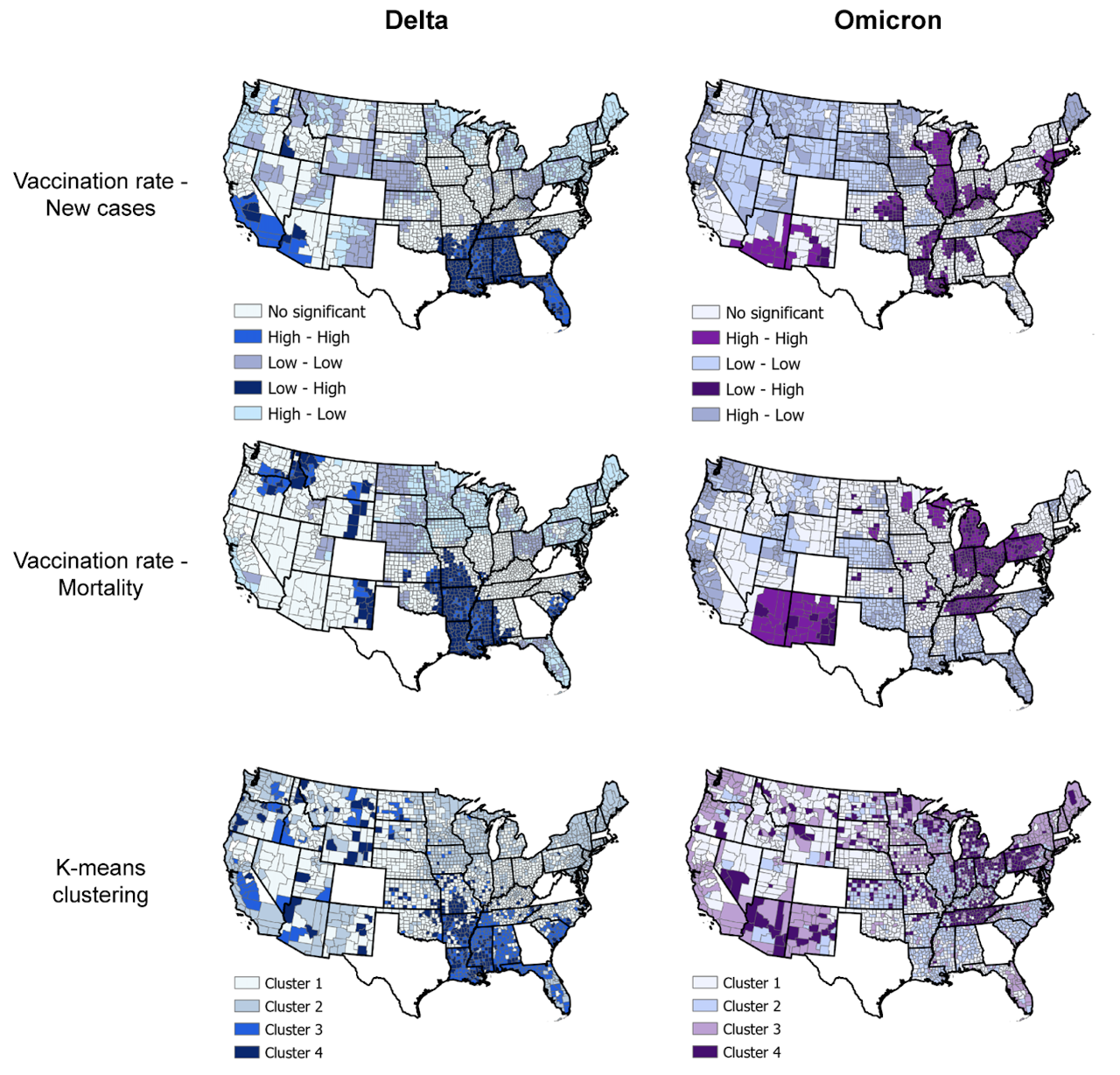
Researchers used county health data to compare the delta and omicron variants of COVID-19. Researchers found that the highly infectious omicron variant spread more quickly in urban, populated areas but caused more fatalities in rural America. Graphic/UC Digital Epidemiology Lab
The epicenter of the omicron wave was concentrated in densely populated, urban counties. But while cases exploded, infections did not lead to the same dire rate of deaths and hospitalizations as previous variants like delta, Cuadros said.
“Delta was less infectious but more deadly than omicron,” Cuadros said.
Despite the lower overall mortality rate among infected patients from omicron compared to earlier variants, unvaccinated people were more than twice as likely to die from COVID-19 as vaccinated patients. Researchers concluded that vaccines make a huge difference in patient outcomes despite the high number of breakthrough cases of omicron among vaccinated patients. As a result, low-vaccination parts of the country, which are mostly rural, continue to bear the highest health burden from the pandemic.
COVID-19 exposed all of these hidden problems in our health care system.
Diego Cuadros, Director of UC's Digital Epidemiology Lab
And researchers worry that rural America will face a disproportionate long-term impact from chronic or lingering symptoms known as long COVID-19.
“We’re talking about an extra burden that rural counties face. They face a higher probability of developing chronic illness from long COVID,” said co-author Claudia Moreno, assistant professor of physiology and biophysics at the University of Washington.

Claudia Moreno
Meanwhile, the ability to track the disease has diminished as fewer people report new cases, which makes it harder for communities to assess their daily risk, Moreno said.
“In the early part of the pandemic, people knew exactly what the infection rates in their counties were day to day — like the weather,” Moreno said. “And now we have peaks in case loads that are so much higher, but there is less public awareness.”
Rural populations are older, which also makes them more vulnerable to COVID-19-related hospitalization and death. Rural America also has fewer doctors and less access to intensive care or ventilators, which are needed to treat complications from COVID-19 infections.
“Rural communities often face many challenges that exacerbate health disparities in the country,” the study concluded. “These areas usually run short on resources, including limited cold chain vaccine storage facilities and health care workers to administer vaccines. The geography can also compound disparities in access that affect rural clinics, which face unique challenges to provide vaccinations to residents who live many miles away.”
Moreno said many people, including herself, know someone who has died from COVID-19. Her cousin’s husband, a basketball coach, died despite his seemingly good health.
“It was devastating to my family,” she said. “That’s why my research has a personal motivation to help the community. You don’t want more families to experience that unnecessary pain.
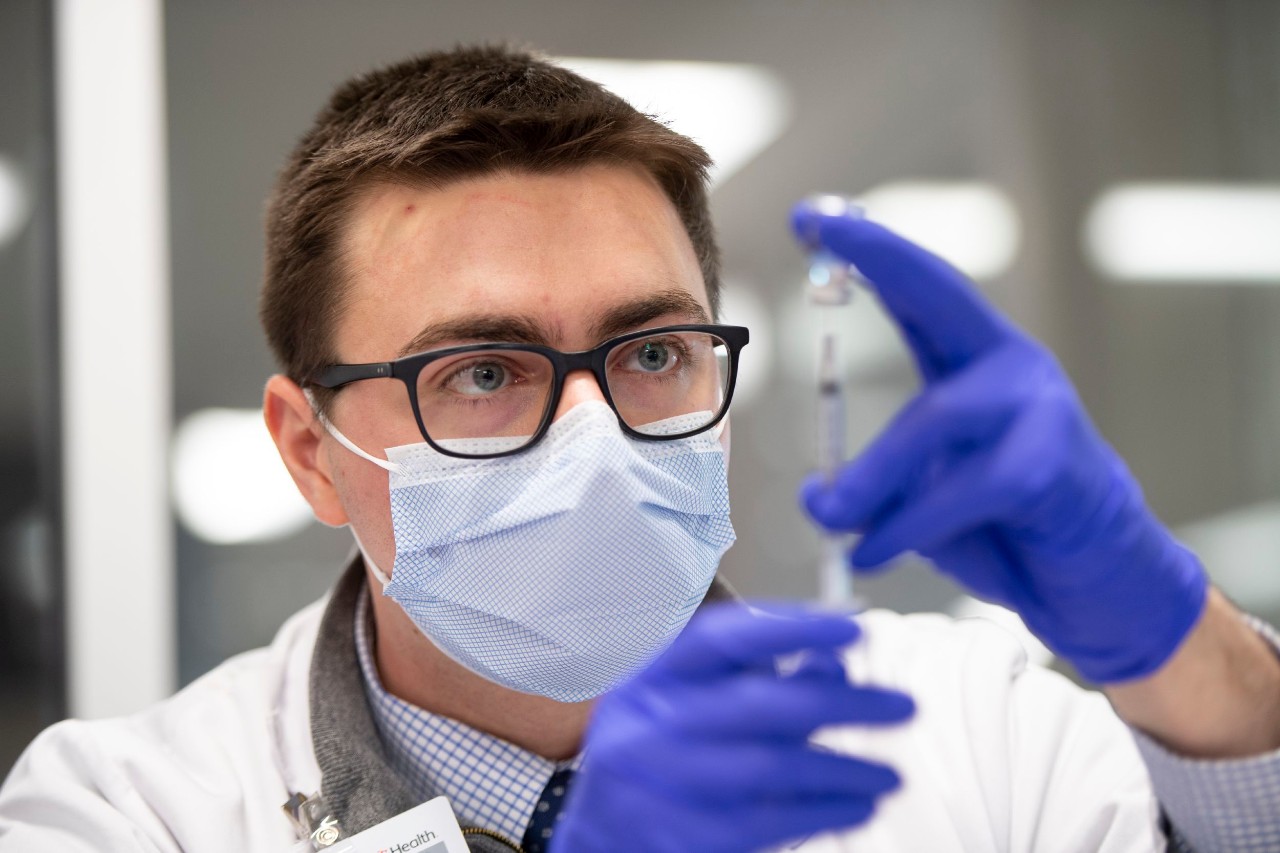
UC College of Pharmacy student Kyle Schuchter draws a COVID-19 vaccine during a drive-through clinic at UC Health in this 2021 file photo. Photo/Colleen Kelley/UC Marketing
“Many of us are getting COVID again and it’s mild,” Moreno said. “But we have to remember the people who died from this disease.”
Researchers say vaccination remains paramount to protect people as the pandemic persists.
“That’s why it’s important to tell people they need to get vaccinated,” Moreno said. “Vaccines work. They’re really helping people prevent death and health complications.”

Diego Cuadros
Cuadros said disparities the study observed have implications far beyond the pandemic.
“COVID-19 exposed all of these hidden problems in our health care system,” Cuadros said.
He has studied the impact of diseases such as AIDS and malaria in developing countries around the world. Ready access to health care makes all the difference, he said.
“We think of the United States as being a rich country with a good health care system, but it’s not true,” he said. “It’s strong in some areas with other areas that are vulnerable with poor access to health care.
“The disparities in rural communities with limited access to health care are invisible. But the pandemic exposed these problems,” he said. “Now that we know about these problems, we can take action to fix them and promote more access to health care in those vulnerable counties.
“From chronic illnesses to opioid addiction — all of these problems will be hitting harder in those same rural areas.” Cuadros said. “We need to start a conversation about how to fix this problem because it’s something we’ll be dealing with for years to come.”
Featured image at top: UC College of Pharmacy student Kaitlin Kuznacic administers a COVID-19 vaccine during a drive-through clinic at UC Health in this 2021 file photo. Photo/Colleen Kelley/UC Marketing
UC researchers respond to COVID-19
UC's research has helped speed vaccine development and delivery, created more effective personal protective equipment and addressed the cascades of social, economic and health impacts of the pandemic. Photo/Fusion Medical/Unsplash
Researchers in colleges across the University of Cincinnati have tackled the COVID-19 pandemic, which has killed more than 6 million people worldwide.
Next Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
Related Stories
UC celebrates record spring class of 2025
May 2, 2025
UC recognized a record spring class of 2025 at commencement at Fifth Third Arena.
UC students recognized for achievement in real-world learning
May 1, 2025
Three undergraduate University of Cincinnati Arts and Sciences students are honored for outstanding achievement in cooperative education at the close of the 2024-2025 school year.
‘Doing Good Together’ course gains recognition
May 1, 2025
New honors course, titled “Doing Good Together,” teaches students about philanthropy with a class project that distributes real funds to UC-affiliated nonprofits. Course sparked UC’s membership in national consortium, Philanthropy Lab.
