Improving treatment for deadly brain tumors
Study finds ChemoID platform-predicted treatments lead to longer survival
New multi-institutional phase 3 clinical trial data published May 2 in Cell Reports Medicine found that a cancer stem cell test can accurately decide more effective treatments and lead to increased survival for patients with glioblastoma, a deadly brain tumor.
The University of Cincinnati’s Soma Sengupta, MD, PhD, a co-first author of the research and a University of Cincinnati Cancer Center physician-researcher, said the research focused on patients whose glioblastoma had returned after initial treatment.
The trial tested the effectiveness of a platform called ChemoID, a CLIA and CAP-accredited diagnostic test, developed by Dr. Pier Paolo Claudio and Dr. Jagan Valluri of Cordgenics LLC.
“ChemoID looks at cancer stem cells and their sensitivity to specified drugs to see which ones will work in a given cancer setting,” said Sengupta, UC associate professor in neurology, director of neuro-oncology clinical trials, associate director of the Brain Tumor Center and a UC Health neuro-oncologist, funded by the Harold C. Schott Endowed Chair in Molecular Therapeutics (Neurosurgery) and the Pam and Tom Mischell Funds.

Soma Sengupta, MD, PhD. Photo/UC Health.
Patients in the trial were randomized to have the choice of chemotherapy treatment decided through ChemoID or to have physicians choose the chemotherapy using standard methods. Sengupta noted oncologists choosing treatments are often dictated by guidelines and insurance considerations.
Those who had their treatments selected through ChemoID had a significantly lower risk of death and, on average, survived 3.5 months longer than those in the physician-choice group.
“We were pleasantly surprised that the ChemoID group did better and that a cancer stem cell-derived test is important in this disease,” Sengupta said. “Where survival in recurrent glioblastoma is extremely poor, 3.5 months or more is wonderful. Some of my patients on this trial are still alive.”
Claudio explained that because ChemoID focuses on choosing treatments using commercially available chemotherapies, this approach offers a way for patients to receive more effective treatment at a lower cost.
Sengupta said the team plans to apply for funding through the National Institutes of Health to develop ChemoID further. A modified platform could expand to include immunotherapy treatments or targeted therapies.
According to Valluri, if the anti-cancer therapy that targets cancer stem cells is incorporated earlier in the treatment plan, ineffective treatments will be eliminated, and patients will be able to receive the maximum therapeutic benefit.
“This is an example of a highly collaborative project,” Sengupta said. “At UC alone, several colleagues, including Dr. Mario Zuccarello and Dr. Rekha Chaudhary, were involved.”
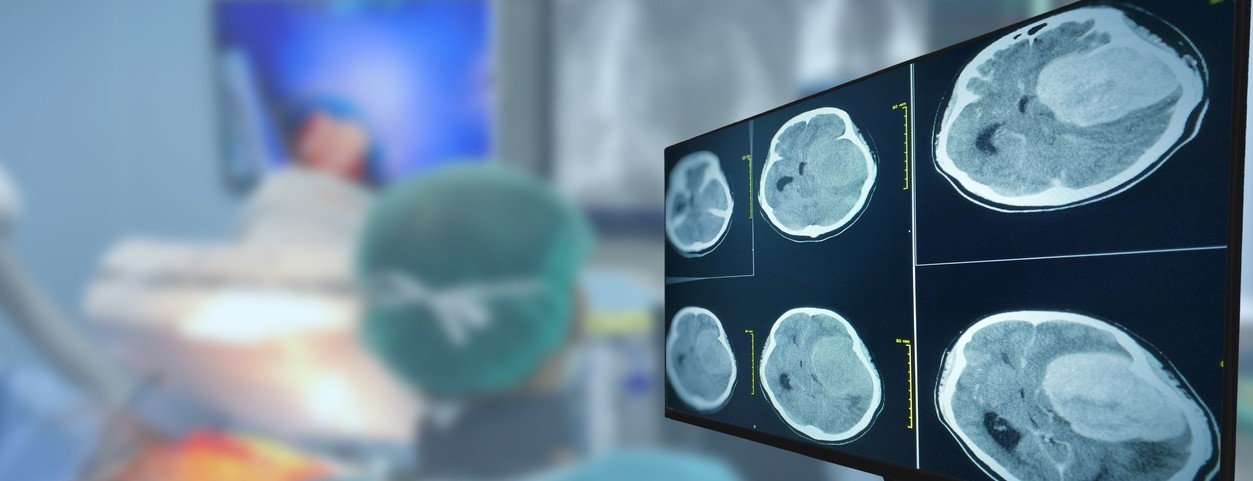
Featured photo at top of a CT brain scan. Photo/Tonpor Kasa/iStock.
Impact Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
Related Stories
Improving treatment for deadly brain tumors
May 5, 2023
The University of Cincinnati's Soma Sengupta was a co-first author on research published in Cell Reports Medicine New that found that a cancer stem cell test can accurately decide more effective treatments and lead to increased survival for patients with glioblastoma, a deadly brain tumor.
Learning more about how cancer affects stroke risk
October 16, 2023
A collaborative team led by University of Cincinnati, University of North Carolina and Duke University researchers is studying how specific cancers and treatments affect patients' risk of stroke.
Collaborative University of Cincinnati Cancer Center team opens Phase 2 brain tumor trial
March 26, 2024
A multidisciplinary team of University of Cincinnati Cancer Center researchers have opened a Phase 2 clinical trial to test a new combination treatment for glioblastomas, the most deadly form of brain tumors.
