Cancer Center experts present research at national conference
Ovarian and blood cancer trials highlight UC’s ASCO abstracts
University of Cincinnati Cancer Center experts will present research at the American Society of Clinical Oncology annual meeting May 31 to June 4 in Chicago.
Platform-predicted treatment leads to longer survival for patients with ovarian cancer

Thomas Herzog, MD. Photo/University of Cincinnati Cancer Center.
After an initial response to chemotherapy, many patients with ovarian cancer encounter a period of resistance to therapy that can lead to tumor regrowth.
The Cancer Center’s Thomas Herzog, MD, said this resistance is believed to be partially caused by cancer stem cells (CSCs) that rebuild and repair tumors after chemotherapy. In a recent trial, researchers used a diagnostic tool called ChemoID that determines how sensitive CSCs and bulk tumor cells are to various cancer-killing therapies.
“The goal of the test is to find the most effective chemotherapeutic agents that would reduce CSCs in ovarian cancer, thereby limiting recurrent disease potential to help improve patients’ outcomes,” said Herzog, a University of Cincinnati Cancer Center member, the Paul and Carolyn Flory Professor in Gynecologic Oncology in the UC College of Medicine, and director of UC Health’s Gynecologic Cancer Disease Center. “ChemoID provides a prioritized list of effective and ineffective chemotherapies after taking a tissue biopsy of the tumor.”
In a multisite clinical trial, patients with recurrent platinum-resistant epithelial ovarian cancer were randomized to have their chemotherapy regimens selected through the ChemoID platform or by their physician’s best choice.
Patients in the physician-choice arm had an overall response rate to their chemotherapy of 5%, while those in the ChemoID arm had a 55% overall response rate. The median progression-free survival, or time after treatment when the disease does not get worse, was three months for the physician-choice group and 11 months for the ChemoID group.
Moving forward, Herzog said a larger trial will be needed to validate these results.
Herzog will present the oral abstract Relationship of cancer stem cell functional assay and objective response rate of patients with recurrent platinum-resistant ovarian cancer in a randomized trial June 1 from 8-9:30 a.m. Co-authors include Thomas Krivak, John Diaz, Scott Lentz, Stephen Bush, Navya Nair, Nadim Bou Zgheib, Camille Gunderson Jackson, Abhijit Barve, Seth Lirette, Candace Howard, Jagan Valluri, Krista Denning and Pier Paolo Claudio.
Herzog will also present the poster Endometrial cancer (EC) by ERBB2 amplification (ERBB2amp) status: Differences in molecular subtypes, ancestry, and real-world outcomes June 3 from 9 a.m. to 12 p.m. Co-authors include Natalie Danziger, Douglas Lin, Julia Elvin, Andrew Kelly, Ryon Graf, Robert Coleman, Bhavana Pothuri, Ramez Eskander, Julia Quintanilha and Brian Slomovitz.
Trial tests drug’s ability to overcome resistance in lymphoma
The Cancer Center’s John Byrd, MD, will present information on a Phase 1 trial testing a new treatment for patients with non-Hodgkin lymphoma (NHL) or chronic lymphocytic leukemia (CLL) whose cancer has returned or stopped responding to treatment (relapsed/refractory).
On average, about a quarter of patients with NHL or CLL will relapse by 24 months. Each patient is unique, and the relapse can occur with different mutations, including a MALT mutation that promotes survival and proliferation of blood cancers.
Cancer cells can also sometimes develop resistance to currently-used drugs targeting other enzymes, creating the need for innovative new therapies.
The trial drug, ONO-7018, targets a protein called MALT1. Preclinical data showed the drug inhibits MALT1 activity and exhibited an antitumor effect with a good safety profile, giving it therapeutic potential to be effective and overcome resistance.

Erin Hertlein, PhD, left, and John Byrd, right, look at data in the Leukemia and Drug Development Lab. Photo/UC Foundation.
In the trial, patients will be given ONO-7018 orally in 21-day treatment cycles. The first group of up to 48 patients will be enrolled to receive increasing doses until the maximum tolerated dose is identified. Once this occurs, a second group of up to 60 patients will be enrolled to receive the optimal dose identified.
“We are excited to have this exciting new agent, ONO-7018, available for our patients with NHL and CLL who have exhausted available effective therapies available for their disease,” said Byrd, Gordon and Helen Hughes Taylor Professor and Chair of the Department of Internal Medicine at the UC College of Medicine. “MALT1 is an exciting target across all B-cell malignancies and potentially for other types of cancer.”
The trial, which is currently recruiting patients, will primarily assess the drug’s safety and tolerability.
Byrd will present the poster A phase I, first-in-human study of ONO-7018 in patients with relapsed/refractory non-Hodgkin lymphoma or chronic lymphocytic leukemia June 3 from 9 a.m. to 12 p.m. Co-authors include Pierluigi Porcu, Thomas Sundermeier, Takashi Nakada, Takeyuki Iwata, Sergio Prados and Leo Gordon.
For more information on this and other blood cancer clinical trials at the Cancer Center, contact Michelle Marcum at marcumma@ucmail.uc.edu or 513-584-6628.
Research examines link between sleep disturbance and cancer-related cognitive impairment
Cancer-related cognitive impairment (CRCI), often called “chemo brain,” affects approximately 75% of individuals with cancer.
The Cancer Center’s cognitive clinical registry found that more than 83% of patients report experiencing sleep disturbances, leading researchers to ask the question of how sleep disturbances and sleep apnea contribute to CRCI.
“CRCI is complex and overlaps with risk factors associated with non-cancer cognitive impairment and neurodegenerative disease,” said Alique Topalian, PhD, a research scientist in Survivorship and Supportive Services at the Cancer Center. “Sleep is central to maintaining brain health. Understanding the relationship between sleep and cancer is important for mitigating CRCI and neurodegenerative disease.”
In patients who do not have cancer, impaired sleep contributes to executive dysfunction and enlarged brain ventricles, which disrupt cerebral spinal fluid (CSF) flow and drainage of waste material from the brain, Topalian said. The team hypothesized this same process may be a contributing factor to CRCI.
“Reduced removal of toxic byproducts of normal brain metabolism and inflammation that is induced by cancer and its treatment could explain one mechanism of action for CRCI and the increased risk of neurodegenerative disease in cancer survivors,” Topalian said.

A Cancer Center team will present findings on how sleep disturbances and sleep apnea affect cancer-related cognitive impairment. Photo/iStock/FG Trade.
The research team analyzed data from 135 patients in the cognitive clinic’s clinical registry and found sleep apnea and sleep disturbances to be highly prevalent in CRCI.
“There was a statistical trend toward a relationship between sleep disturbance severity in CRCI and enlarged ventricles,” Topalian said. “Sleep disturbances did not correlate with measures of cognitive impairment. However, ventricular size was significantly associated with impaired processing speed, sustained attention/inhibitory control and semantic fluency.”
Topalian said the novel finding of enlarged brain ventricles in these patients suggests treatment aimed at improving sleep disturbances may help regulate disrupted CSF flow, which could potentially improve CRCI cognitive symptoms.
“We are pursuing fundings for a CPAP and sleep health treatment trial for CRCI patients to investigate how treatment impacts cognitive, imaging and serum markers of CSF flow,” she said.
Additionally, the research team plans to form an ongoing translational working group to expand research on this topic.
Research assistant Sophie Kushman will present the poster “Sleep apnea and glymphatic dysfunction as a mediator of executive dysfunction and neurodegenerative risk in cancer related cognitive impairment (CRCI)” during the Symptom Science and Palliative Care session June 3 from 1:30 to 4:30 p.m. Abstract co-authors are Topalian and Rhonna Shatz, DO.
Unique approach aids elementary science education
As the University of Cincinnati Cancer Center is tackling how to reduce the suffering and mortality of cancer in the community today, it is also testing unique ways to encourage the next generation of cancer researchers.
William Barrett, MD, co-director of the Cancer Center, professor and chair of Radiation Oncology in UC’s College of Medicine, and medical director of the Barrett Center for Cancer Prevention, Treatment and Research, said elementary students, particularly those in socially and financially disadvantaged settings, encounter barriers to effective scientific learning.
With an aim to overcome these barriers, which include maintaining interest, concentration and focus, Barrett and his colleagues implemented a scientific educational program for children attending an urban community center’s after-school program.
During the program’s activities, five students at a time complete three-minute sessions at tutoring stations on human physiology, astronomy, geography, geology and cancer led by medical students or residents. Meanwhile, another group of five students goes through three-minute basketball drills with a coach on the court.

Cancer Center volunteers developed a scientific educational program that alternated basketball drills with educational stations at a community center's after-school program. Photo/Nik Shuliahin/Unsplash.
The groups alternate between basketball and tutoring until all students have participated in all five drills and tutoring stations. Then the kids are quizzed on what they learned, and an end-of-practice scrimmage begins with a score based on the quiz results.
“Within weeks, nearly every child could list the planets of the solar system in order; calculate their pulse and explain its importance; list the most common symptoms of the most prevalent cancers; correctly identify continents, oceans, countries and states on maps; and explain the origin of volcanoes, earthquakes, hurricanes and tsunamis,” Barrett and his coauthors wrote in the abstract.
The alternating of physical exertion with learning appears to maintain interest, focus and concentration, and the approach could be widely applied to students from diverse backgrounds.
Barrett is first author on the abstract Defeating cancer through education, prevention, and youth athletics. Sherwin Anderson, Andrew Frankart, Samuel Thompson and William Mackey are co-authors.
Impact Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
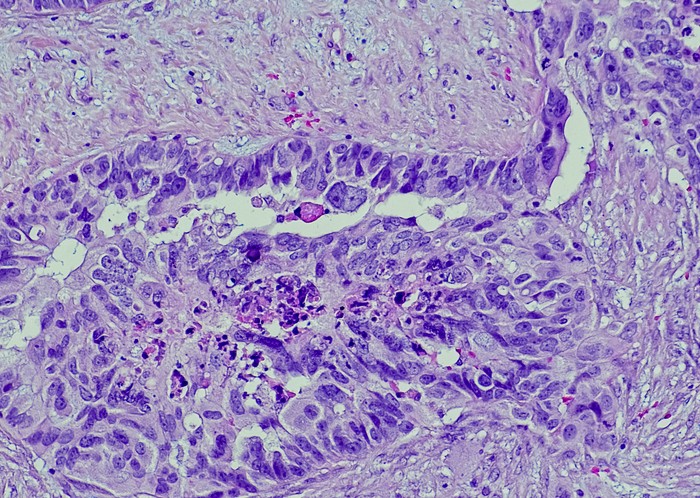
Featured photo at top of ovarian cancer cells. Photo/OGPhoto/iStock.
Related Stories
Cancer Center experts present research at national conference
May 29, 2024
University of Cincinnati Cancer Center experts will present research on ovarian and blood cancer trials, the link between poor sleep and cancer-related cognitive impairment, and an innovative youth education program at the American Society of Clinical Oncology annual meeting 2024 in Chicago.
A potential new treatment for brain tumors
September 23, 2022
The University of Cincinnati's Pankaj Desai, PhD, has received a $1.19 million grant from the National Institutes of Health/National Institute of Neurological Disorders and Stroke to continue research into the use of a drug called letrozole to treat glioblastomas, the most deadly form of brain tumors.
Learning more about how cancer affects stroke risk
October 16, 2023
A collaborative team led by University of Cincinnati, University of North Carolina and Duke University researchers is studying how specific cancers and treatments affect patients' risk of stroke.
