Head and neck, cervical cancer and meningioma research highlights of UC ASTRO abstracts
Cancer Center researchers to present at national meeting
University of Cincinnati Cancer Center experts present research at the American Society for Radiation Oncology (ASTRO) Annual Meeting Sept. 29 through Oct. 2.
Osteoradionecrosis more common in patients with head and neck cancer that requires partial jaw removal

Alyssa Farley, MD. Photo/University of Cincinnati.
Following radiation treatment for head and neck cancer, some patients can experience osteoradionecrosis (ORN) when an area of exposed bone fails to heal after a three-month period.
“ORN of the mandible and maxilla (jaw bones) can be very debilitating, as it often causes severe pain, fistula formation, infection and susceptibility to fractures,” said Alyssa Farley, MD, a third-year resident in the Department of Radiation Oncology in UC’s College of Medicine. “The symptoms directly and indirectly from ORN lead to a significant decrease in quality of life for patients, including severe financial burdens.”
Farley and her colleagues — including Vinita Takiar, MD, PhD, who is principal investigator on the project — looked at contemporary rates for ORN in oral cavity squamous cell carcinoma, a specific type of head and neck cancer.
In this subpopulation, the team found higher rates of ORN than previously reported. Rates of ORN increased as age at diagnosis decreased and when surgical removal of part or all of the mandible or maxilla was part of the treatment plan.
ORN management can range from conservative medications to intense surgical intervention, Farley said. Moving forward, the team plans to study preventative treatments in identified high-risk populations to decrease ORN rates.
Coauthors of the abstract include Takiar, Farley, Nigel Dick and Taylor Petery.
Progesterone contraception a risk factor for visual impairment in patients with meningiomas

Morgan Bailey, MD. Photo provided.
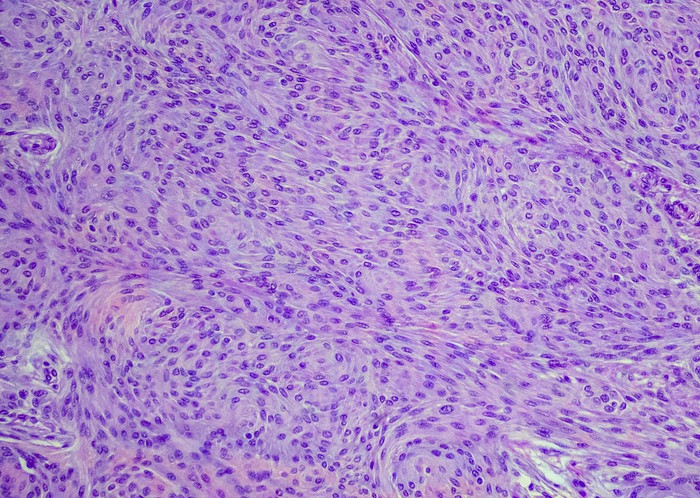
Brain or spinal cord tumors called meningiomas can cause visual impairment, which is sometimes severe and permanent, that can be used as a surrogate for analyzing tumor growth.
In theory, the estrogen and progesterone receptors on these meningiomas could help the tumors grow when exposed to higher levels of these hormones. However, a lack of data prevented further understanding of how hormonal contraception affected tumor growth in premenopausal women with meningiomas being referred for radiation.
“We wanted to understand the connection and risk of taking hormonal contraception/supplementation to vision deficits related to meningiomas,” said abstract first author Morgan Bailey, MD, a resident in the Department of Radiation Oncology in UC’s College of Medicine.
The researchers found progesterone — specifically the drug formulation Provera — is a significant risk factor for meningioma-related vision loss in this patient population. They are now performing testing on all patient samples to see how many patients express the progesterone receptor.
“We have contacted women from our study taking these medications to inform them of the risk, many of whom have since stopped taking Provera,” Bailey said. “Our findings highlight the importance of age-appropriate counseling, consistent pathologic assessment of estrogen receptor/progesterone receptor status for meningiomas and a greater awareness of the risk of meningioma-related vision loss amongst neurosurgeons and radiation oncologists.”
Additional coauthors include senior author Kyle Wang, Chase Avery, Luke Pater, Tim Struve, Ralph Vatner, Andrew Frankart, Sarah Sittenfeld, Kevin Shiue, Lalanthica Yogendran, Rekha Chaudhary, Jonathan Forbes, Norberto Andaluz, Matthew Hagen, Ady Kendler, Rocco Rossi and John Breneman.
Radiation and Plk1 inhibitor a potential combination therapy for HPV-negative head and neck cancer

Julianna Korns, UC doctoral student. Photo provided.
Researchers analyzing patient and clinical trial data have found current frontline treatments for head and neck cancer are insufficient to improve survival outcomes on their own, presenting the need to develop combination therapies that attack cancer cells on multiple fronts.
Cancer Center researchers have focused on a specific gene called Plk1 that, when high, typically correlates with lower survival rates and is known to be overexpressed in many cancers, including head and neck cancers.
“The main research question we were asking was to investigate the role of Plk1 in head and neck cancer patients,” said abstract first author Julianna Korns, a doctoral student working in Takiar and Trisha Wise-Draper’s lab. “We wanted to determine if targeting Plk1 with a highly specific inhibitor, onvansertib, would enhance radiation therapy for head and neck cancer patients.”
Korns explained head and neck cancers can be broken down by human papillomavirus (HPV) status. HPV-negative patients are typically more resistant to therapy than HPV-positive patients.
The team found combining onvansertib with radiation treatment reduced the cell viability and tumor growth of HPV-negative head and neck cancers but did not have the same effect on HPV-positive cancer cells.
“We are currently investigating the mechanistic differences between HPV-negative and HPV-positive head and neck cancers after treatment with onvansertib and radiation,” Korns said. “Overall, we have promising data that points to combining Plk1 inhibition by using onvansertib and radiation in HPV-negative head and neck cancer patients that we hope will translate into clinical trials in this patient population.”
Coauthors of the abstract include Takiar, Korns, Wise-Draper and Maria Lehn.
Treatment, outcomes for geriatric patients with cervical cancer match younger patients

Sarah Feldkamp, MD. Photo/University of Cincinnati.
Historical national trends have found that treatment patterns for geriatric (age 65 and older) patients with cervical cancer differ compared to younger patients. A Cancer Center research team examined treatments and cancer-related outcomes for geriatric patients with cervical cancer compared to younger patients treated at UC.
First author Sarah Feldkamp, MD, said the team found treatment patterns for geriatric patients at UC match those of younger counterparts.
“We also found no differences in cancer specific mortality, recurrence rates or overall survival between the younger and older age cohorts,” said Feldkamp, a resident in the Department of Radiation Oncology in UC’s College of Medicine. “This is also in contrast to outcome trends seen on a national level, suggesting that more conservative treatment patterns may be responsible for historically disparate outcomes.”
Feldkamp said she plans to additionally examine differences in toxicity outcomes between the two age cohorts treated at UC when writing a full manuscript on her findings.
Additional abstract coauthors include Teresa Meier and Sarah Sittenfeld.
Impact Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
Cancer Center researchers’ involvement at ASTRO includes:
- Teresa Meier, MD, moderating the special session “Developmental Therapies and Quality Assurance in Early Phase Gynecologic Clinical Trials,” Sept. 29 at 8 a.m.
- Vinita Takiar, MD, PhD, participating as a mentor in the session “Navigating and Maximizing the Mentor-Mentee Relationship,” Sept. 29 at 3 p.m.
- Emily Daugherty, MD, comoderating the session “Exploring the Future of AI, Radiomics and Deep Learning in Radiation Oncology Research,” Sept. 29 at 4:45 p.m.
- Sarah Feldkamp, MD, presenting the poster “Treatment Patterns and Outcomes in Geriatric Women with Cervical Cancer,” Sept. 30 at 8 a.m.
- Anthony Mascia, PhD, presenting “Proton Flash Trials: Insights from FAST-01 and 02,” Sept. 30 at 10:45 a.m.
- Morgan Bailey, MD, presenting the poster “Progesterone Contraception Is Associated with Tumor-Related Visual Impairment in Premenopausal Women with Meningioma Referred for Radiation,” Sept. 30 at 10:45 a.m.
- Jonathan Sackett, MD, presenting the poster “Rapid Early Progression After Surgery for IDH-Wildtype Glioblastoma and the Importance of the Pre-Radiation Planning MRI,” Sept. 30 at 10:45 a.m.
- Luke Pater, MD, presenting the invited speaker discussion “Current Radiotherapy Approaches for Pediatric Wilms Tumor,” Sept. 30 at 3 p.m.
- Julianna Korns, BS, presenting the poster “Combining Plk1 Inhibition and Radiation to Target Head and Neck Cancer,” Sept. 30 at 5 p.m.
- Takiar moderating the education session “Prophylactic Feeding Tube Placement in Head and Neck Cancer: Hard to Swallow?” Oct. 1 at 2:30 p.m.
- Maddie Schumacher, BS, presenting the poster “Toxicity After Proton Beam Therapy for New and Recurrent Breast Cancer,” Oct. 2 at 8:30 a.m.
- Alyssa Farley, MD, presenting the poster “Osteoradionecrosis Incidence in Oral Cavity Squamous Cell Carcinoma,” Oct. 2 at 10:30 a.m.
Featured photo at top of meningioma cells. Photo/OGphoto/iStock.
Related Stories
Head and neck, cervical cancer and meningioma research highlights of UC ASTRO abstracts
September 30, 2024
University of Cincinnati Cancer Center experts present research at the American Society for Radiation Oncology (ASTRO) Annual Meeting Sept. 29 through Oct. 2.
Lattice therapy can help target tumors
August 19, 2024
Rio Grande Valley, Texas news station KRGV-TV highlighted University of Cincinnati Cancer Center researcher Andrew Frankart's new trial testing lattice therapy to provide more targeted radiation for patients with large tumors.
Cancer Center researcher studies combination therapy to improve leukemia treatment
September 6, 2024
The University of Cincinnati Cancer Center’s Eric Vick, MD, PhD, has been awarded a nearly $215,000 grant from the Leukemia and Lymphoma Society (LLS) and a $50,000 American Society of Clinical Oncology (ASCO) Young Investigator Award to continue research into a combination therapy treatment for acute myeloid leukemia (AML).
