Trial Uses Genetic Test to Tailor Breast Cancer Treatment
CincinnatiResearchers believe a genetic test used to calculate a womans risk for breast cancer recurrence may also help determine if a subset of patients would be better off with less aggressive therapy following surgery.
According to Jennifer Manders, MD, it is not always clear which follow-up treatmentchemotherapy, hormone therapy or a combination of bothis most effective for women who fall into the gray area of intermediate risk for breast cancer recurrence.
Currently, many patients with early stage breast cancer are given both hormones and chemotherapy to control recurring tumor growth and kill any residual cancer cells in the body.
Research suggests, however, that chemotherapy could have no measurable benefit to patients with less-aggressive cancers whose risk for recurrence is unclear.
A major phase-3 trial, led locally by surgeons Elizabeth Shaughnessy, MD, PhD, and Manders, is underway to investigate whether hormone therapy alone can produce better cancer-free survival for women who fall into the intermediate recurrence risk category.
Research tells us that giving hormone therapy alone to women at low risk for recurrence and chemotherapy followed by hormonal therapy to women at a high risk for recurrence makes medical senseits the women who fall in the middle that were unclear about, explains Manders, an assistant professor at the University of Cincinnati (UC).
We need to develop a method of tailoring follow-up treatment that addresses the specific characteristics of a patients tumor, she adds. This will allow us to more accurately predict what medical treatments will be most effective at alleviating the disease long term.
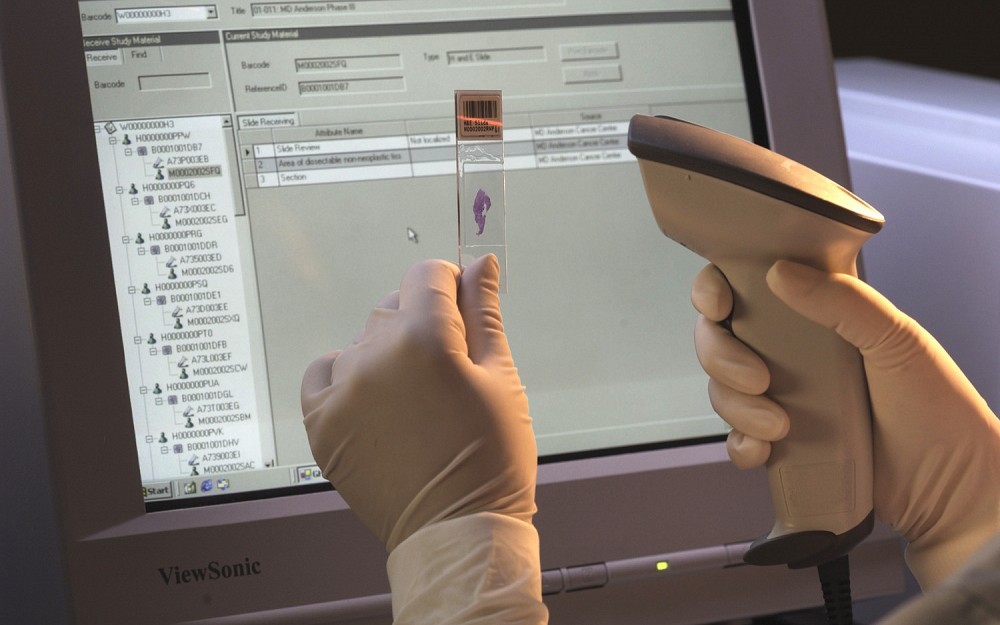
This National Cancer Institute-sponsored trialknown as TAILORxuses genetic tests to obtain an individualized and quantitative analysis of how likely a specific patients breast cancer is to recur.
When a patient enrolls in the trial, a tumor tissue sample is sent to a central processing lab where scientists analyze it against a panel of 21 genes with known links to breast cancer.
Using a statistical risk prediction model, the scientists then calculate a score that represents the specific patients risk for breast cancer recurrence. The score is determined from the gene expression results using a range of zero to 100. Scores between 11 and 25 are considered to be in the intermediate or unclear risk category this trial focuses on.
Manders says information gathered from the genetic breast cancer test could give physicians a better understanding of the specific characteristics of their patients breast tumors, which is critical in planning accurate treatment plans and follow-up.
This trial asks: will the majority of women in that moderate risk group will benefit from chemotherapy, hormonal therapy or a combination of both? says Manders. If we can answer that question, we can customize treatment based on a tumors specific characteristics and apply more logical medical regimens that minimize unnecessary treatmentand the correlating potential side effects.
Study participants are placed into one of four treatment arms, based on their recurrence scores. Women considered at low risk (10 or less) will receive hormone therapy, with women on the other end of the scale (26 or more) will get both chemotherapy and hormone therapy. The remaining women falling into the intermediate risk group will be randomized to receive either hormone therapy alone or a combination of chemotherapy plus hormone therapy.
Women who have undergone surgery for localized stage 1 or 2 hormone receptor-positive breast cancer may be eligible for the trial.
Some insurance providers, including Medicare, provided coverage for genetic testing. Patients who qualify for this trial will receive the genetic testing and corresponding treatment visits at no cost.
For enrollment information, call Ruth Steele at (513) 584-2951.

Jennifer Manders, MD, is a breast surgeon and assistant professor of medicine at the University of Cincinnati.

Elizabeth Shaughnessy, MD, PhD, specializes in the treatment of breast diseases.
Tags
Related Stories
UC study: Brain organ plays key role in adult neurogenesis
July 2, 2024
The University of Cincinnati has published research in the Proceedings of the National Academy of Sciences that found the choroid plexus and cerebrospinal fluid play a key role in maintaining a pool of newly born neurons to repair the adult brain after injury.
Put down that beer; it's not a tanning lotion
July 1, 2024
The University of Cincinnati's Kelly Dobos joined WVXU's Cincinnati Edition to discuss what's fact and what's myth when it comes to sunscreen use, different kinds of sunscreen and a social media recommendation to use beer on your skin to help get a tan.
Cincinnati researchers want to know if MRIs can work better
June 28, 2024
WVXU and the Cincinnati Business Courier highlighted a new collaboration between the University of Cincinnati College of Medicine, UC Health GE HealthCare, JobsOhio, REDI Cincinnati and Cincinnati Children’s to create an MRI Research and Development Center of Excellence located on UC’s medical campus.
