Surgically Implanted Radiation Seeds May Reduce Cancer Recurrence
CINCINNATIA multidisciplinary University of Cincinnati (UC) team is testing whether tiny radioactive seeds implanted during surgery can reduce the recurrence of lung cancer.
The study could open up a new treatment option for patients currently considered too ill to undergo the standard surgical approach.
The clinical trial will compare minimally invasive lung surgery with the same surgery combined with cancer-killing radioactive seeds (brachytherapy) in high-risk patients with early non-small-cell cancer, one of the two major forms of lung cancer.
Standard care for patients with early non-small-cell lung cancer is a lobectomy, the surgical removal of the entire lobe (or lobes) of the lung and surrounding lymph nodes.
However, says Sandra Starnes, MD, assistant professor of surgery and principal investigator of the Cincinnati arm of the national phase-3 study, some patients already have extremely reduced lung function, and other serious medical conditions that make them poor candidates for the surgery.
For this trial, the researchers will perform a less-extensive surgeryknown as a sublobar section or extended wedge resectionto remove the cancerous lung tissue and a small margin of normal lung tissue around the tumor.
We hope that by pairing wedge resection surgery with targeted radiation therapy, which is delivered from inside the body, well be able to reduce cancer recurrence in these patients while maintaining their quality of life, said Kevin Redmond, MD, associate professor of radiology and study coinvestigator.
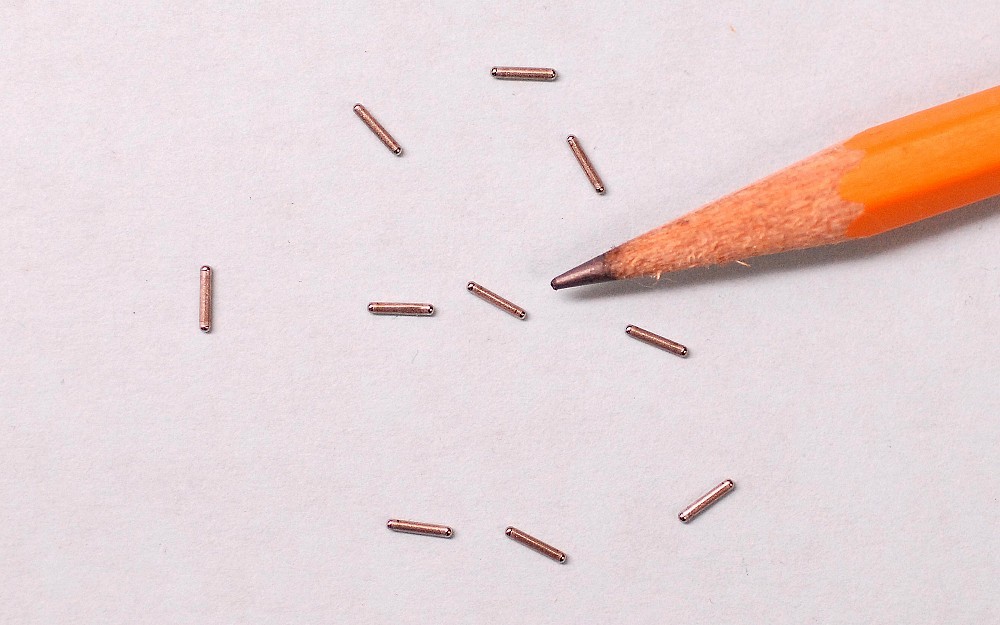
Encased in titanium, the radiation seeds are just 5 millimeters long and no wider than the tip of a paperclip. The seeds are implanted along the suture line during surgery to deliver targeted radiation from inside the body over about six months.
Redmond says brachytherapy has been used in prostate cancer for about 20 years and is currently being testing in other cancers, including brain and breast cancer.
Too many patients are declared ineligible for surgery and denied a potentially curative procedure because they werent evaluated by a surgeon who specializes in this type of cancer, adds Starnes. In reality, many patients with early-stage, non-small-cell lung cancers could get the care they need to beat early lung cancer if they were seen by a multidisciplinary thoracic oncology team.
Nationally, researchers are looking for about 226 patients with stage-1, non-small-cell lung cancer. Patients will be randomized to have only lung surgery or surgery plus brachytherapy.
Cancer status will be verified by biopsy prior to surgery. Patients will also undergo a pulmonary function test (breathing exercises) and complete a quality-of-life survey before and after surgery.
Following treatment, researchers will track cancer recurrences for three years through periodic computed tomography (CT) scans of the chest and upper abdomen.
According to the American Cancer Society, more than 185,600 people will be diagnosed with non-small-cell lung cancer in 2007. It is the leading cause of cancer-related deaths in the United States. Although the most common form of the disease, non-small- cell lung cancer is typically less aggressive than small-cell lung cancer, the second major type of lung cancer.
For eligibility information on this trial, sponsored by the American College of Surgeons Oncology Group, call Alison Kastl at (513) 584-0436.

Sandra Starnes, MD, is a thoracic surgeon who specializes in mediastinal tumors and minimally invasive lung surgery.
Tags
Related Stories
Growing heart failure epidemic calls for prioritizing primary...
May 5, 2025
A rapidly growing heart failure epidemic calls for prioritizing primary prevention, according to a new scientific statement from the American Heart Association published in Circulation in April. The statement reviews the current evidence for predicting heart failure risk and offers risk-based strategies for heart failure prevention.
Machine learning brings new insights to cell’s role in...
April 30, 2025
Researchers led by the University of Cincinnati’s Anna Kruyer and the University of Houston’s Demetrio Labate have published research in the journal Science Advances applying object recognition technology to track changes in brain cell structure and provide new insights into how the brain responds to heroin use, withdrawal and relapse.
Most teens prescribed SSRIs did not have recommended follow-up...
April 30, 2025
The University of Cincinnati and Cincinnati Children's Hospital Medical Center's Martine Lamy commented to Medscape on new research that found fewer than half of the adolescents prescribed a selective serotonin reuptake inhibitor (SSRI) at two large Chicago pediatric primary care clinics had a follow-up visit within the recommended 6 weeks.
