Clinical Trial Offers Different Option for Locally Advanced Pancreatic Cancer Treatment
CINCINNATIIndividuals with locally advanced pancreatic cancer who are not eligible for surgery have an investigational treatment option that combines chemotherapy with radiation therapy in a novel sequence not currently used to treat locally advanced pancreatic cancer.
The drugs and the radiation technique are not newbut the combination and sequence of use is: chemotherapy followed by chemoradiation then further chemotherapy. University of Cincinnati (UC) Cancer Institute clinician-scientists leading the trial say this could be a key difference in making therapy more effective.
According to the National Cancer Institute, nearly 44,000 people will be diagnosed with pancreatic cancer in 2013. Five-year survival rates among both men and women are less than 6 percent.
The pancreas is responsible for producing juices that aid in food digestion and certain hormones that help control blood sugar and store energy. Because of the organs locationbehind the stomach, in front of the spineand lack of clear symptoms or warning signs, pancreatic cancer often goes undetected until it has reached an advanced stage.
In this new UC-investigator initiated and sponsored clinical trial, the multidisciplinary gastrointestinal cancer team will test a two-drug chemotherapy regimen given in conjunction with dose-escalated radiation therapyknown as intensity modulated radiation therapy (IMRT). Previously, patients with locally advanced pancreatic cancer would have received standard radiation therapy at lower doses.
Led locally by Michelle Mierzwa, MD, and Olugbenga Olowokure, MD, the UC trial is currently open through the UC Cancer Institute at UC Health clinical facilities, including the UC Health Barrett Center in Clifton and UC Health Physicians Office South in West Chester. About 50 patients are expected to enroll.
"Surgery is the only potential cure for pancreatic cancer. The challenge is that many patients come to us when their tumor has grown so large that surgery is unsafe or ineffective due to its proximity to other organs and major blood vessels, explains Olowokure, a UC Health medical oncologist and an assistant professor in the UC College of Medicine Department of Internal Medicine, Division of Hematology Oncology. "Our job is to try to shrink the tumor to a size that makes surgery a viable option while also doing everything we can to achieve cancer control and prolong survival.
Clinical Trial Treatment
In this phase-2 clinical study, all participants will receive trial drugs and radiation. Treatment starts with two chemotherapy drugsnab-paclitaxel and gemcitabinegiven weekly (three weeks on, one week off).
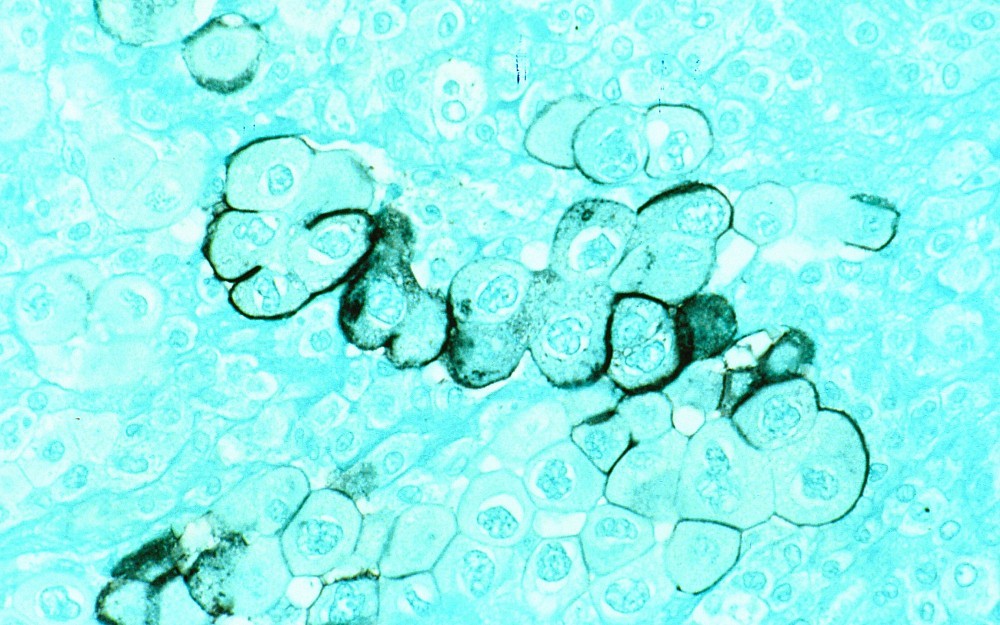
Gemcitabine (marketed as Gemzar) is an anti-metabolite drug that stops growth of cancer cells by preventing the cells from making DNA and RNA. The drug is approved by the Food and Drug Administration (FDA) for the treatment of pancreas, breast, ovarian and lung cancer.
Nab-paclitaxel (marketed as Abraxane) is an anti-microtubule agent thought to work by inhibiting the microtubule structures within the cell, ultimately resulting in cell death. It is currently FDA-approved for treatment of locally advanced lung cancer and recurrent/metastatic breast cancer, but is being testing in other cancers, including metastatic pancreatic cancer. In this clinical trial, both drugs will be given on days 1, 8 and 15 of a four-week cycle.
Animal studies have shown that nab-paclitaxel may also block an enzyme called cytidine deaminase (CDA), which normally destroys the drug gemcitabine being used to destroy the tumor.
"By using the agents in combination, we hope to increase the amount of gemcitabine getting into the pancreatic tumor, thereby making gemcitabine more effective at killing the cancer cells, says Olowokure.
After completion of two cycles of chemotherapy, study participants will have IMRT for six weeks given consecutively with a weekly infusion of gemcitabine. Trial treatment concludes with two additional four-week cycles of chemotherapy (three weeks on, one week off) using the nab-paclitaxel/gemcitabine combination.
"Although radiation therapy is an important part of pancreatic cancer treatment, we have traditionally used lower doses of radiation to minimize side effects to the surrounding healthy tissues in the small intestine, stomach, kidneys and spinal cord, explains Mierzwa, a UC Health radiation oncologist and assistant professor in the UC College of Medicine Department of Radiation Oncology. "With IMRT, we are able pinpoint size and shape each radiation treatment beam down to a few millimeters, which gives us more precise treatment at higher dosages.
Preliminary Data
UC initial data has shown that this novel combination of drugs and sequence of therapy has potential to increase treatment effectiveness.
A retrospective review of the UC Cancer Institute gastrointestinal team patient database showed that 38 percent of patients with locally advanced pancreatic cancer treated with the nab-paclitaxel/gemcitabine combination were able to undergo resection. Overall survival of the entire group was 85 percent at six months and 77 percent at 12 months. Mierzwa and Olowokure presented these findings at the American Society of Clinical Oncology meeting in June 2012.
Clinical Trials Information
To learn more, call the UC Cancer Institute Clinical Trials Office at 513-584-7698 or visit uccancer.com/clinicaltrials.

Michelle Mierzwa, MD

Olugbenga Olowokure, MD
Related Stories
The latest efforts in cervical cancer prevention
May 12, 2025
Medical Laboratory Observer interviewed the University of Cincinnati Cancer Center's Leeya Pinder to discuss the current state and future of cervical cancer prevention.
Study links adverse childhood experiences to higher risk of...
May 12, 2025
Children who have been exposed to adverse childhood experiences face an increased risk of homelessness during their childhood, according to a new study from a researcher in the University of Cincinnati’s School of Social Work.
Ohio could soon make breast cancer screenings more affordable
May 9, 2025
The University of Cincinnati Cancer Center's Ann Brown was featured in Local 12 and Cincinnati Enquirer reports on a bill introduced by Rep. Jean Schmidt in the Ohio legislature that seeks to eliminate out of pocket medical expenses such as copays and deductibles associated with supplemental breast cancer screenings.
