UCMC Uses Watchman and Decision Analytic Model to Assist AF Patients
Mark Unger, 57, initially wondered if a history of pneumonia along with outdoor heat and activity from his work in construction were making breathing so difficult.
None of these scenarios were the case. When a simple run left him exhausted, a trip to the emergency room followed, and soon, after some much desired answers. Unger was diagnosed with atrial fibrillation (AF), an irregular often rapid heart rhythm that leads to poor circulation. It was 2004, and Unger was still fairly young for a condition more likely to affect older patients.
What followed during the next decade were a series of surgeries involving catheter ablation, a minimally invasive procedure that allows physicians to destroy small areas in the heart that are misfiring and causing atrial fibrillation, followed with treatment using anticoagulants such as Warfarin or Coumadin.
Two ablations were conducted by Alexandru Costea, MD, UC Health cardiologist and director of the Center for Electrophysiology, Rhythm Disorders and Electro-Mechanical Interventions. Unger, of Laurelville, Ohio, says he found the anticoagulants were rough on his system.
"A lot of people call it rat poison, says Unger, referring to Warfarin. "Its so hard to eat around it. Too much vitamin K in your diet will make the medication drop in your system. You have to be dedicated, and it was like figuring out a Rubics Cube for me. It made me feel cold. My mother had to take Warfarin, and I thought she was imagining things when she complained, but it does make you feel cold.
Costea recommended Unger as a candidate for implantation of the Watchman device, a left atrial appendage (LAA) implant developed by Boston Scientific and designed to decrease the risk of stroke in atrial fibrillation patients. It serves as an alternative for AF patients who need blood-thinning medication but are not good candidates for taking it long-term for instance, because of a high risk of bleeding, says Costea, a professor at the University of Cincinnati College of Medicine.
The Watchman consists of a delivery catheter inserted through the patients groin and a parachute-shaped device that expands and covers the left atrial appendage. It has been proven that this is where most clots that cause AF-related strokes develop.
Unger says his surgery was completed in August 2017 and his warfarin was then discontinued. Hes very pleased with his recuperation and ability to be more active. "UC Medical Center is a true blessing, says Unger. "It is a great facility and great nursing care. Its a top-notch hospital. The cardiac unit there is fantastic.
Costea says other hospitals in the region and beyond use the Watchman, but UC Medical Center finds its outcomes with the device are more successful because of its use of the Atrial Fibrillation Decision Support Tool (AFDST), a computerized decision analytic model integrated into UC Healths electronic health record.
The AFDST allows UC Health to standardize its program for treating AF patients and takes the guess work out of treatment, says Costea.
"There is a very clear algorithm of people who benefit from the Watchman and of people who dont, says Costea.
Mark Eckman, MD, UC Health physician and director of the Division of General Internal Medicine at the UC College of Medicine, developed the AFDST, which pulls information about AF patients from the electronic health record and is able to calculate for the individual patient his or her risk of AF-related stroke and major bleeding while taking blood thinning therapy. Based on this information, the AFDST makes suggestions for the best treatment to prevent AF-related stroke.
The decision support tool uses the patients age, gender and history of stroke or bleeding, along with whether the individuals had vascular disease, a history of myocardial infarction, alcoholism, intracranial hemorrhage, hypertension, congestive heart failure, abnormal liver and other health aliments. The model estimates the patients life expectancy, adjusted by quality-of-life for each possible treatment based on these characteristics and offers a recommendation along with guidelines on treatment of atrial fibrillation from the American College of Cardiology/American Heart Association/Heart Rhythm Society.
"There is a risk of major bleeding on blood thinning therapy, and the tool basically delivers a recommendation based on the balance of risk and benefit indicating whether a patient on average would do better with blood thinning therapy versus without, says Eckman.
Costea says he may recommend the Watchman for a patient, but a second physician must independently review a patient and also conclude the device is a necessity. Its a requirement from the U.S. Food and Drug Administration.
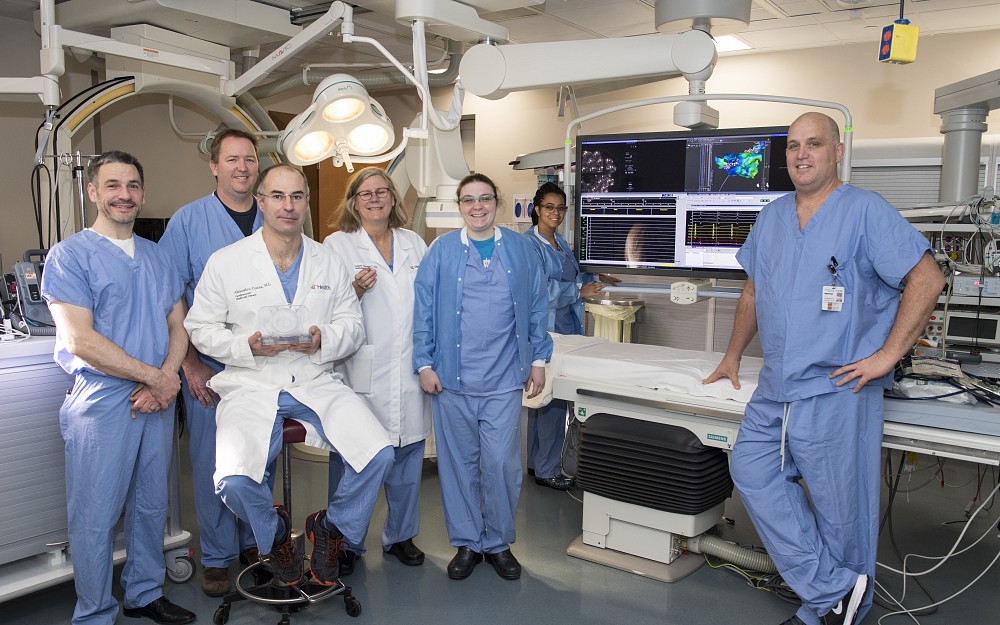
Physicians trained in implantation of the Watchman also have the support of a team of medical professionals in the areas of cardiac anesthesia, interventional cardiology, transesophageal echocardiography and cardiac surgery at UC Medical Center, says Costea.
For more information about atrial fibrillation call UC Health at 475-8521.

Mark Unger is enjoying life again after UC Medical Center physicians successfully implanted a Watchman Device. He is shown in the UCMC lobby.

Mark Eckman, MD, director of the Division of General Internal Medicine, is shown in the UC College of Medicine.
Related Stories
UC researcher launches app to connect patients to lifesaving...
May 7, 2025
A cardiologist and researcher at UC’s College of Medicine joined the Venture Lab at the 1819 Innovation Hub to launch High Enroll, an app that links clinical trials with willing participants.
Study explores social media’s growing influence on cosmeceutical...
May 7, 2025
The University of Cincinnati's Kelly Dobos spoke with Cosmetics Design USA about new research that revealed a significant rise in consumer interest in cosmeceuticals, or cosmetic products with active ingredients purported to have medical benefits.
UC, UC Health see frontline student training as workforce...
May 6, 2025
Amid ongoing challenges across the health care workforce, including burnout and shortages, the University of Cincinnati is working to tackle this issue through a program that embeds students in clinical settings.
